Journal of Vita Columbia Volume 2 Issue 1 – Clinical Nutrition
Zinc: A Synopsis of this Critical Trace Mineral
January 18th, 2022
How to cite this article:
Azer M, Azer M, Magsakay CR. Zinc: A Synopsis of this Critical Trace Mineral. 2022. Journal of Vita Columbia. 2(1).
Abstract:
Zinc is one of the most crucial and most abundant minerals in the human body. Like most minerals, its deficiency leads to non-specific signs and symptoms. While it is common though, it is crucial to the immune system of the body and its deficiency and toxicity can lead to hazardous states which may be catastrophic in one’s health.
Introduction:
Zinc is the second most abundant trace mineral in the human body after iron, and is present in every cell. (1) Zinc can be found in many animal and plant food sources, but its highest levels exist in shellfish, salmon, lobster, beef, pork, lamb, chicken, milk and milk products, eggs, lentils, beans, oats, peas, asparagus and mushrooms. (1) However, zinc from animal products is absorbed more efficiently than from plant-based products. (1)
The Role of Zinc in the Human Body
- Zinc has an important role in gene expression, DNA and protein synthesis (1).
- It aids in over 300 enzymatic reactions in digestion, nerve function and other metabolic reactions. (1) It also aids in immune function (1)
- Zinc aids in collagen synthesis so it plays a crucial role in having a healthy skin and wound healing. In fact, skin has about 5% of zinc content in the human body. (1)
- It’s used in growth and development (1)
- It also has anti-inflammatory effect (1)
- Zinc plays an essential role in bone formation and health (5)
- Zinc may significantly reduce risk of age-related diseases, such as pneumonia, infection and age-related macular degeneration (AMD). (1)
- It’s important to maintain healthy vision. (2)
- It also acts significantly in blood clotting (2)
- It improves thyroid function (2)
Zinc Deficiency:
Some groups are more at risk of zinc deficiency than others, such as sickle cell anemia patients (1), those with eating disorders (bulimia or anorexia) (1), patients with chronic kidney disease (1), people with alcohol abuse disorder (1), vegetarians and vegans. (1) Pregnant and lactating females (1), those with poor dietary intake (1), liver cirrhosis (2), gastrointestinal diseases (inflammatory bowel disease, short bowel syndrome, malabsorption (3), older infants (7-12 months old) who are exclusively breastfed (3), diabetes (3) and those with malignancy (3) are also susceptible to zinc deficiency.
It is estimated that around 2 billion people worldwide are deficient in zinc due to inadequate dietary intake. (1) Symptoms of mild zinc deficiency include diarrhea, decreased immunity, thinning hair, decreased appetite, mood disturbances, dry skin, fertility issues and impaired wound healing (1). In severe zinc deficiency, there is impairment in growth and development, delayed sexual maturity, skin rashes, chronic diarrhea, generalized hair loss, impaired wound healing, poor sense of taste and smell, irritability and behavioral changes (1, 2). Severe deficiency can also impair the immune system as it can depress neutrophils, macrophages and complement activity. (3) Also, it decreases lymphocytes proliferation and activation. This results in increased risk of pneumonia and other infections especially in extremes of age (3).
Since zinc deficiency impairs immune system function, it’s thought to cause over 450,000 deaths in children under 5 every year (1). In truly severe cases, it can also lead to acute diarrhea which is a significant cause of mortality among children in developing communities (3).
Treatment of Zinc Deficiency
The treatment for zinc deficiency is fairly simple. Firstly, the recommended daily dose is 11 mg for men and 8 mg for women (except pregnant and lactating who need around 14-19 mg daily). If a higher dose is needed, it should be recommended and monitored by physicians only; however, the daily dose should not exceed 40 mg to avoid toxicity. (2) The National Institutes of Health consider 40 mg of zinc a day to be the upper limit dose for adults and 4 mg of zinc a day the upper limit for infants under age 6 months. (4) The preferred means of administration are zinc citrate and zinc gluconate as these forms are more easily absorbed. (1)
Clinical Uses of Zinc:
There are several uses of zinc. Zinc is commonly used in hospitals as a treatment for burns, ulcers and other skin injuries. Also, for uncontrolled acute childhood diarrhea the World Health Organization and UNICEF recommend short-term zinc supplementation (20 mg of zinc per day, or 10 mg for infants under 6 months, for 10–14 days) (3). Many studies have even confirmed that zinc supplementation may improve many conditions such as Wilson’s disease, diabetes mellitus, depression, ADHD, macular degeneration, leprosy, warts, acne and gingivitis (2).
Zinc Toxicity:
Zinc toxicity can occur due to ingestion of 100 m daily or taking high doses for many consecutive years, this can double the risk of prostate cancer (2). Ingestion of 10 gm of zinc at once can be fatal (2).
Acute symptoms of zinc toxicity include GIT upset (nausea, vomiting, diarrhea, loss of appetite and abdominal cramps) and headaches. (1) A more chronic effect of zinc toxicity is a decline in HDL levels. (1)
Pharmacologic Interactions with Zinc:
A potential problem with zinc treatment however is that zinc supplements can interfere with other medications (2). For example, they decrease the absorption of some antibiotics like tetracycline sans quinolones. (2) Zinc supplements can also interfere with the absorption and action of penicillamine, decreasing its effect (3).
Taking high amounts of zinc can also affect the absorption of other nutrients such as copper and iron (1). Zinc can increase the effect and the side effects of cisplatin. (2) On the other hand, zinc can be affected by medication, for example some diuretics such as thiazides increase urinary excretion of zinc, decreasing its level in blood. (3)
Conclusion:
In conclusion zinc is required for life, while in deficiency states it may be easy to treat, zinc toxicity can lead to various signs and symptoms, up to and including cancer. Like many minerals that are used by the body, symptoms are vague and non-specific; however, there are certain key signs to look for, such as an impaired immune system, that elucidates the possibility of zinc deficiency.
References:
- The Nutrition Source – Selenium., Harvard T.H. Chan – School of Public Health., https://www.hsph.harvard.edu/nutritionsource/selenium/
- Raman, Ryan., 10 Signs and Symptoms of Iodine Deficiency., Healthline Nutrition, Nov. 2017., https://www.healthline.com/nutrition/iodine-deficiency-symptoms
- Navarro-Alarcon M, Cabrera-Vique C. Selenium in food and the human body: a review. Sci Total Environ. 2008 Aug 1;400(1-3):115-41. doi: 10.1016/j.scitotenv.2008.06.024. Epub 2008 Jul 26. PMID: 18657851. https://pubmed.ncbi.nlm.nih.gov/18657851/
- Mangiapane E, Pessione A, Pessione E. Selenium and selenoproteins: an overview on different biological systems. Curr Protein Pept Sci. 2014;15(6):598-607. doi: 10.2174/1389203715666140608151134. Erratum in: Curr Protein Pept Sci. 2018;19(7):725. PMID: 24910086.
- Kang, D., Lee, J., Wu, C. et al. The role of selenium metabolism and selenoproteins in cartilage homeostasis and arthropathies. Exp Mol Med 52, 1198–1208 (2020). https://doi.org/10.1038/s12276-020-0408-y
- Jenkins DJA, Kitts D, Giovannucci EL, Sahye-Pudaruth S, Paquette M, Blanco Mejia S, Patel D, Kavanagh M, Tsirakis T, Kendall CWC, Pichika SC, Sievenpiper JL. Selenium, antioxidants, cardiovascular disease, and all-cause mortality: a systematic review and meta-analysis of randomized controlled trials. Am J Clin Nutr. 2020 Dec 10;112(6):1642-1652. doi: 10.1093/ajcn/nqaa245. PMID: 33053149; PMCID: PMC7727482. https://pubmed.ncbi.nlm.nih.gov/33053149/
- Selenium – Fact Sheet for Health Professionals., National Institutes of Health- Office of Dietary Supplements., March 2021., https://ods.od.nih.gov/factsheets/Selenium-HealthProfessional/
- Shi, Ying., Yang, Wei., Tang, Xianwen., Keshan Disease: A Potentially Fatal Endemic Cardiomyopathy in Remote Mountains of China., Frontiers in Pediatrics – Pediatric Cardiology., March 2021., https://www.frontiersin.org/articles/10.3389/fped.2021.576916/full
- Schepman, Karin., Engelbert, Raoul., Kashin Beck Disease: more than just osteoarthrosis., National Institutes of Health, U.S. National Library of Medicine., June 2010., https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3080494
- Moghaddam A, Heller RA, Sun Q, Seelig J, Cherkezov A, Seibert L, Hackler J, Seemann P, Diegmann J, Pilz M, Bachmann M, Minich WB, Schomburg L. Selenium Deficiency Is Associated with Mortality Risk from COVID-19. Nutrients. 2020 Jul 16;12(7):2098. doi: 10.3390/nu12072098. PMID: 32708526; PMCID: PMC7400921. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7400921/
- Selenium,., WebMD – Vitamins and Supplements., https://www.webmd.com/vitamins/ai/ingredientmono-1003/selenium
- Thomas, Liji., Selenium Toxicity., News – Medical Life Sciences., April 2021., https://www.news-medical.net/health/Selenium-Toxicity.aspx
- Selenium., Medsafe – New Zealand Medicines and Medical Devices Safety Authority., July 2000., https://www.medsafe.govt.nz/profs/puarticles/sel.htm
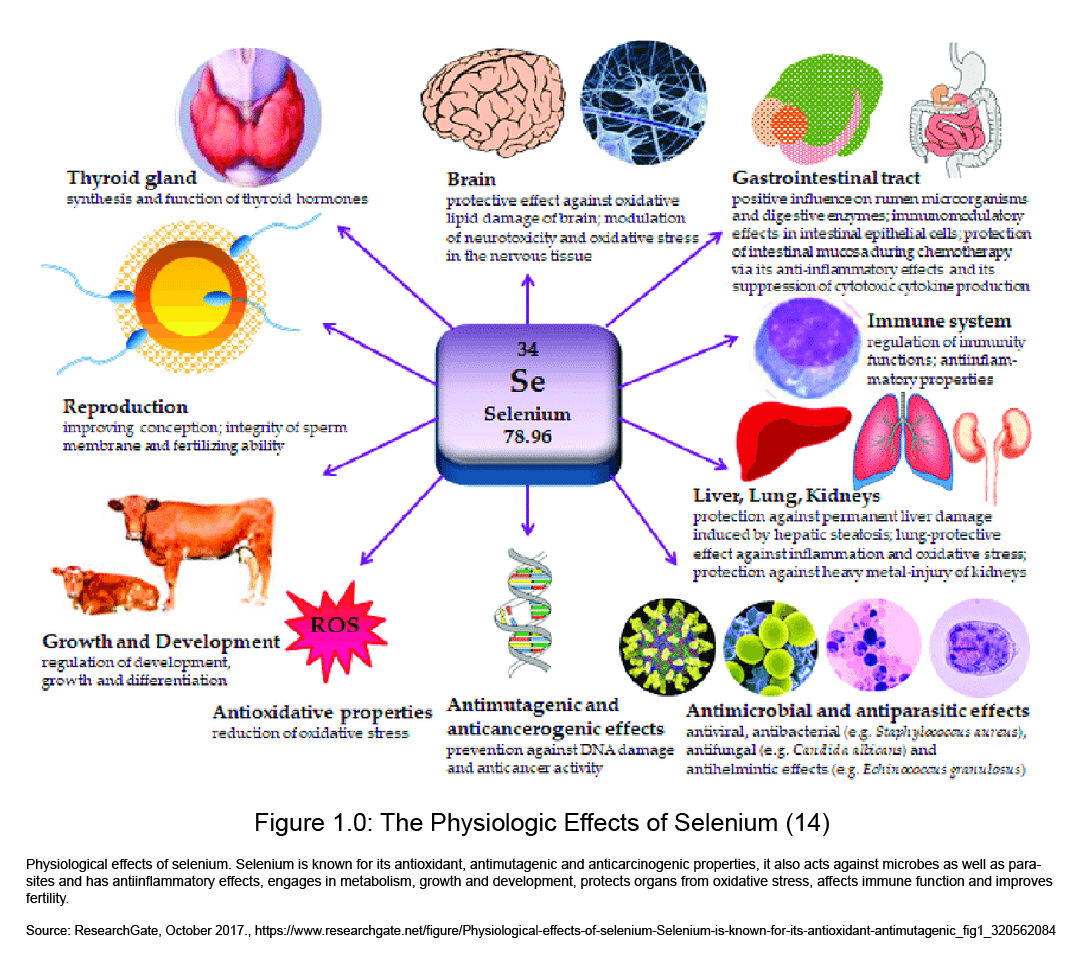
- picture reference: ResearchGate, October 2017., https://www.researchgate.net/figure/Physiological-effects-of-selenium-Selenium-is-known-for-its-antioxidant-antimutagenic_fig1_320562084